Let’s do Zone 2
Zone 2 Exercise and Metabolic Health
Zone 2 exercise has received growing attention for its potential benefits to metabolic health, and I’m a huge fan. Personally, it’s easier for me to commit to a Zone-2-ish brisk walk than a more vigorous workout like running. In Nature Wants Us to Be Fat, Dr. Richard J. Johnson (2022) recommends endurance-type exercise in Zone 2—about one hour, three or four times per week—to support mitochondrial health. The goal, as described in the book, is to keep exercise intensity around 70% of maximum heart rate, below the threshold where lactate begins to accumulate.
What Is Zone 2 Training?
Practically speaking, Zone 2 corresponds to roughly 60–70% of your maximum heart rate, often called a “conversational pace” (American College of Sports Medicine [ACSM], as cited in Elder, 2023; Cleveland Clinic, 2025). At this level, you should be able to maintain conversation but not sing.
There is some question, however, about whether this intensity is vigorous enough. Recent research indicates that while Zone 2 training is beneficial, it may not be uniquely optimal for mitochondrial or cardiorespiratory adaptations; higher-intensity intervals can sometimes yield greater benefits in less time (Storoschuk et al., 2025). Still, for many people, the accessibility and sustainability of Zone 2 activity make it a practical cornerstone of long-term metabolic health.
Physical Activity Guidelines for Americans
According to the Physical Activity Guidelines for Americans (U.S. Department of Health and Human Services [HHS], 2018), adults should engage in 150–300 minutes of moderate-intensity aerobic activity per week, or an equivalent combination of moderate and vigorous exercise, to achieve substantial health benefits and lower the risk of chronic disease.
Moderate-intensity activity is defined as 3.0–5.9 METs on an absolute scale or about a 5–6 on a 0–10 perceived-exertion scale. In practical terms, this is an effort level where a person can talk but not sing.
HHS also created the Move Your Way campaign to help Americans apply these guidelines in daily life.
The “Active Couch Potato” Problem
Even when people meet weekly exercise recommendations, too much sitting can diminish the benefits. The term “active couch potato” describes individuals who exercise regularly yet spend most of their day sedentary (Owen et al., 2010; Dunstan et al., 2012).
Prolonged sitting—eight or more hours daily—has been linked to impaired glucose regulation and lipid metabolism, independent of structured exercise. I relate to this personally: during years of doing vigorous HIIT workouts, I’d often spend hours afterward sitting at my desk.
To counter these effects, research suggests adding short movement breaks throughout the day—standing, stretching, or walking for a couple of minutes every 30–60 minutes—to improve metabolic flexibility and reduce sedentary time.
Balancing Strength and Aerobic Training
The key takeaway: we need to move, and likely more than most of us do. Regular movement supports health and helps prevent metabolic dysfunction, but it’s not just about weight loss.
A growing social media narrative claims that strength training is more important than aerobic exercise. In truth, both are essential. Strength training builds muscle mass and metabolic resilience, while aerobic exercise supports cardiovascular and mitochondrial health.
The best approach is to create realistic, individual activity goals that can be maintained over time.
Measuring Activity: Understanding METs
If you’re looking for ways to assess or diversify your physical activity, the Compendium of Physical Activities from Arizona State University’s Healthy Lifestyles Research Center is a valuable tool. It lists hundreds of activities with their corresponding MET values—from sleeping (0.9 METs) to intense running (18 METs).
MET stands for Metabolic Equivalent of Task and represents the energy cost of physical activity relative to resting.
1 MET = energy expenditure while sitting quietly, roughly equal to consuming 3.5 mL of oxygen per kilogram per minute, or about 1 kcal/kg/hour.
Examples:
Light activity: < 3 METs (slow walking, light chores)
Moderate activity: 3–5.9 METs (brisk walking, gardening)
Vigorous activity: ≥ 6 METs (running, fast cycling)
The Compendium allows users to browse activities by type—household, recreational, or occupational—and compare MET values to national guidelines for a more informed fitness strategy.
Final Thoughts
Zone 2 exercise offers an accessible, sustainable way to support metabolic and mitochondrial health, especially when combined with other forms of movement and reduced sedentary time. Ultimately, consistency matters most: find the balance of aerobic and strength activities that fits your life, and keep moving regularly for long-term wellness.
Disclaimer
This content is for general educational purposes and should not replace individualized medical or exercise advice. Always consult a qualified healthcare professional before starting a new fitness or training program.
References
Johnson, R. J. (2022). Nature wants us to be fat: The surprising science behind why we gain weight and how we can prevent—and reverse—it. BenBella Books. (See exercise recommendation: sustained ≥1 hour, 3–4×/week.)
Storoschuk, K. L., Moran-MacDonald, A., Gibala, M. J., & Gurd, B. J. (2025). Much ado about Zone 2: A narrative review assessing the efficacy of Zone 2 training for improving mitochondrial capacity and cardiorespiratory fitness in the general population. Sports Medicine, 55(7), 1611–1624. https://doi.org/10.1007/s40279-025-02261-y PubMed
Cleveland Clinic. (2025). Exercise heart rate zones explained (Zone 2 ≈ 60–70% HRmax). Cleveland Clinic
American College of Sports Medicine (via Elder, 2023). Moderate intensity ≈ 64–76% HRmax. Technologies, 11(3), 66.
U.S. Department of Health and Human Services. (2018). Physical Activity Guidelines for Americans (2nd ed.). U.S. Department of Health and Human Services. https://health.gov/paguidelines
Dunstan, D. W., Howard, B., Healy, G. N., & Owen, N. (2012). Too much sitting—a health hazard. Diabetes Research and Clinical Practice, 97(3), 368–376. https://doi.org/10.1016/j.diabres.2012.05.020
Owen, N., Healy, G. N., Matthews, C. E., & Dunstan, D. W. (2010). Too much sitting: The population-health science of sedentary behavior. Exercise and Sport Sciences Reviews, 38(3), 105–113. https://doi.org/10.1097/JES.0b013e3181e373a2
U.S. Department of Health and Human Services. (n.d.). Move Your Way. https://health.gov/MoveYourWay/
Ainsworth, B. E., Herrmann, S. D., Jacobs Jr., D. R., Whitt-Glover, M. C., Tudor-Locke, C., & Barreira, T. V. (2024). The Compendium of Physical Activities (Adult, Older Adult & Wheelchair versions). Arizona State University Healthy Lifestyles Research Center. https://pacompendium.com/
Ainsworth, B. E., Haskell, W. L., Herrmann, S. D., Meckes, N., Bassett, D. R., Tudor-Locke, C., ... & Leon, A. S. (2011). 2011 Compendium of Physical Activities: A second update of codes and MET values. Medicine & Science in Sports & Exercise, 43(8), 1575–1581. https://doi.org/10.1249/MSS.0b013e31821ece12
.
Leptin and Weight Management
Leptin
Ever Heard of Leptin?
Ever heard of leptin? It’s a hormone that plays a critical role in regulating your appetite, energy levels, and body weight. 🌟
Leptin is often referred to as the satiety hormone because it signals your brain when you’ve had enough food, helping you feel full after eating. However, when leptin levels are out of balance, they can contribute to increased hunger, overeating, and weight gain. 🤯
Leptin’s Role in Metabolism
Leptin is produced by fat cells and communicates with the brain — particularly the hypothalamus — to regulate appetite and energy expenditure.
High leptin levels signal that you have sufficient fat stores, which should reduce appetite.
Low leptin levels can trigger hunger and lead to overeating or weight gain.
Basically, leptin is the hormone that should be saving us from excessive energy intake — from overeating. When it’s working properly, leptin helps regulate appetite, energy use, and body weight. In many ways, it may be the key to a properly functioning weight management system.
Why Weight Management Shouldn’t Be So Hard
It’s common sense to think that maintaining a healthy weight shouldn’t be so difficult. We weren’t meant to count calories or track every macro. No other animal in nature does that to stay at its ideal weight. Sure, some animals have metabolic challenges, but most maintain a consistent, stable body composition naturally.
Humans, on the other hand, put enormous effort into measuring, restricting, and managing — yet we remain the species most prone to weight fluctuations and metabolic struggles. So what gives?
Leptin Resistance: When the Body Stops “Listening”
Since leptin is the hormone that helps prevent overeating, a natural first question might be: “Why don’t I produce enough leptin?”
But for most people, that’s not the issue. In many cases, despite having plenty of fat stores, the body becomes resistant to leptin’s signals — a condition known as leptin resistance. This can lead to chronic hunger, overeating, and difficulty losing weight. The real problem is that the brain and cells stop responding to leptin. The signal that should say “you’ve had enough” no longer gets through.
Leptin resistance is often linked to metabolic conditions such as obesity, insulin resistance, and chronic inflammation.
Leptin Resistance and Metabolic Health
Leptin resistance can create a feedback loop that makes managing appetite and energy balance even harder. The body interprets the lack of signal as starvation, increasing hunger and slowing metabolism. Over time, this pattern can contribute to weight gain, fatigue, and metabolic dysfunction — even when calorie intake isn’t excessive.
How to Improve Leptin Sensitivity
Eat a balanced diet: Focus on whole foods, healthy fats, lean proteins, and fiber to support healthy leptin function.
Move regularly: Physical activity improves leptin sensitivity and overall metabolic health.
Manage stress: Chronic stress disrupts hormonal balance and can impair leptin signaling.
Prioritize sleep: Poor sleep alters leptin and ghrelin levels, increasing hunger and cravings.
Restoring Balance
This is one example of why Rebase Wellness aims to take a systems-based approach to well-being — recognizing that hormones like leptin are part of a larger network influencing energy, metabolism, and mindset. Weight gain or difficulty losing weight is not a moral failure or a lack of willpower. It’s a signal that something in the system is out of balance. Sustainable change rarely comes from a single strategy, like calorie restriction; it requires understanding and addressing the interconnected factors that support metabolic health and long-term wellness.
Metabolic Syndrome - America’s Public Health Crisis
What Is Metabolic Syndrome and Why It Matters
Do you have metabolic syndrome? Even if you’ve never heard the term, it’s possible that you may be experiencing it — in fact, there’s a significant chance. According to the National Heart, Lung, and Blood Institute (2022), “metabolic syndrome is common in the United States. About 1 in 3 adults have metabolic syndrome.”
Unfortunately, in addition to one in three adults, a growing number of children are also affected by this health-impacting condition.
Defining Metabolic Syndrome
Metabolic syndrome has been recognized for decades, though its definition has evolved. In 2009, several major health organizations — including the American Heart Association and the National Heart, Lung, and Blood Institute — collaborated to create a unified definition of metabolic syndrome (MetS). This remains the clinical standard used today (Alberti et al., 2009).
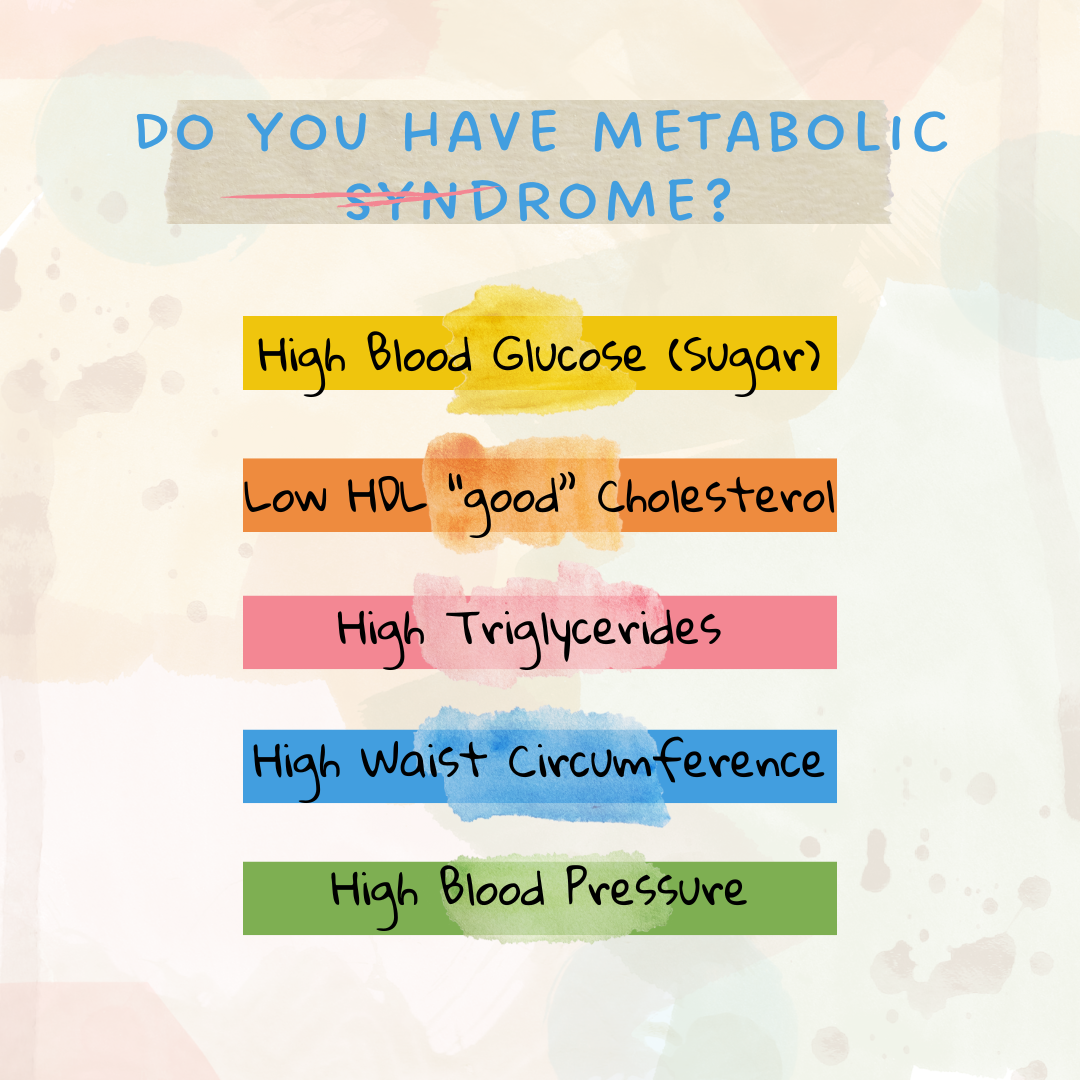
According to these guidelines, metabolic syndrome can be diagnosed when an individual has three or more of the following conditions (Alberti et al., 2009):
High blood glucose (blood sugar)
Low HDL (“good”) cholesterol
High triglyceride levels
Large waist circumference
High blood pressure
Why Metabolic Syndrome Is a Public Health Concern
Metabolic syndrome is a serious health issue in both adults and children. Its importance lies not only in its direct impact but also in its strong connection to other chronic diseases — particularly heart disease and type 2 diabetes (Alberti et al., 2009).
Given its growing prevalence, metabolic syndrome is now considered a major public health concern. To reverse this trend, we would need to see clear evidence that rates are declining across the population. Despite ongoing research, awareness campaigns, and preventive health efforts, a large-scale solution remains elusive. Still, continued education, early detection, and lifestyle support are critical for improving outcomes.
References
Alberti, K. G. M. M., Eckel, R. H., Grundy, S. M., Zimmet, P. Z., Cleeman, J. I., Donato, K. A., Fruchart, J.-C., James, W. P. T., Loria, C. M., & Smith, S. C., Jr. (2009). Harmonizing the metabolic syndrome: A joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation, 120(16), 1640–1645. https://doi.org/10.1161/CIRCULATIONAHA.109.192644
National Heart, Lung, and Blood Institute. (2022, May 18). What is metabolic syndrome? U.S. Department of Health and Human Services. https://www.nhlbi.nih.gov/health/metabolic-syndrome